Insights
3 November 2015
6 cognitive tests for research of depression and mood disorders
Mood disorders affect 5-10% of the adult population in a given year. The most common mood disorders are major depressive disorder, dysthymia, and bipolar disorder. Here we explore the six CANTAB tests for objectively measuring cognitive function in depression.
Mood disorders affect 5-10% of the adult population in a given year1, 2. The most common mood disorders are major depressive disorder, dysthymia, and bipolar disorder. Collectively, mood disorders cause considerable distress to affected individuals, and can have a devastating impact on quality of life and everyday functioning. In the World Health Organization’s Global Burden of Disease study, depression was second only to ischaemic heart disease in terms of associated disability3.
Patients with depression will frequently report subjective cognitive slowing, or difficulty in concentrating, in addition to depressed mood. Indeed, research has shown that objectively measured cognitive dysfunction is present in depression, affecting a number of different domains4,including memory, attention and executive function. Some of these deficits persist following remission, potentially impacting occupational function even after an improvement in mood. Current research is attempting to target these cognitive symptoms of depression. For example, a recent study at the University of Cambridge looking at modafinil, a compound usually used to treat narcolepsy, to improve areas of impaired cognitive functioning in depression.
CANTAB has a six test battery specially designed to assess cognition in studies of depression and associated mood disorders for both academic research and clinical trials.
One touch stockings of Cambridge
What does it test?
OTS is a test of executive function, spatial planning and working memory based upon the Tower of Hanoi test.
What does the task involve?
 The participant is shown two displays of coloured balls held in stockings suspended from a beam. There is a row of numbered boxes along the bottom of the screen. The participant is asked to solve problems by working out how they would move the balls in the bottom display in order to make them match the arrangements of the ball sin the top display. After some training and practice problems, the participant is asked to work out in their head how many moves the solutions to these problems require, and then touch the appropriate box at the bottom of the screen to indicate their response.
The participant is shown two displays of coloured balls held in stockings suspended from a beam. There is a row of numbered boxes along the bottom of the screen. The participant is asked to solve problems by working out how they would move the balls in the bottom display in order to make them match the arrangements of the ball sin the top display. After some training and practice problems, the participant is asked to work out in their head how many moves the solutions to these problems require, and then touch the appropriate box at the bottom of the screen to indicate their response.
Why this test
Patients with mood disorders often experience difficulties in executive functions such as planning: these can be assessed using the OTS task4.
Delayed Matching to Sample
What does it test?
DMS assesses forced choice recognition memory for non-verbalisable patterns, testing both simultaneous matching and short term visual memory.
What does the task involve?
 This test assesses visual matching ability and visual recognition memory. The participant is shown a complex visual pattern and then after a brief delay, four patterns. The participant must touch the pattern that matches the sample. In some trials the sample and the choice patterns are shown simultaneously, whereas in others there is a delay (of 0, 4 or 12 seconds) before the four choices appear.
This test assesses visual matching ability and visual recognition memory. The participant is shown a complex visual pattern and then after a brief delay, four patterns. The participant must touch the pattern that matches the sample. In some trials the sample and the choice patterns are shown simultaneously, whereas in others there is a delay (of 0, 4 or 12 seconds) before the four choices appear.
Why this test
Patients presenting with depression often show signs of forgetfulness or memory deficits. DMS is sensitive to these impairments, and can be used to assess changes over time in response to interventions.
Emotion recognition task
What does it test?
ERT measures the ability to identify emotions in facial expressions. Subjects choose between six basic emotions.
What does the task involve?
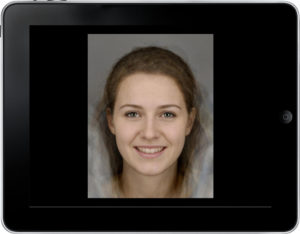 Computer morphed images derived from the facial features of real individuals each showing a specific emotion, are displayed on the screen, one at a time. Each face is displayed for 200ms and then immediately covered up, and participant must select which emotion the face displayed from 6 options.
Computer morphed images derived from the facial features of real individuals each showing a specific emotion, are displayed on the screen, one at a time. Each face is displayed for 200ms and then immediately covered up, and participant must select which emotion the face displayed from 6 options.
Why this test
Those who suffer from depression have been shown to provide more negative ratings of emotional expressions5, 6, 7. This reflects the well-known negative bias seen in depression, where positive or neutral stimuli are seen as more negative. The brief presentation encourages implicit processing, as opposed to conscious appraisal of the faces.
Spatial Working Memory
What does it test?
SWM looks at how good participants are at retaining and utilising visuospatial information. It is self-ordered and since participants must employ a strategy it also provides insight into executive function.
What does the task involve?
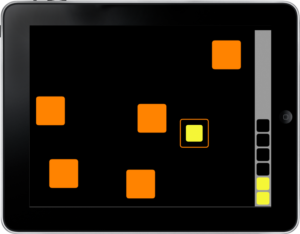 An array of coloured boxes contain tokens which participants must search for by touching the boxes. The number of boxes increases, making the task more difficult. Crucially, participants must not return to a box in which they have previously found a token.
An array of coloured boxes contain tokens which participants must search for by touching the boxes. The number of boxes increases, making the task more difficult. Crucially, participants must not return to a box in which they have previously found a token.
Why this test
Studies have shown that patients with depression have moderate impairments in working memory4. Working memory is a critical cognitive skill for a range of everyday tasks.
Rapid Visual Information Processing
What does it test?
RVP tests how well participants can sustain their visual attention and how they cope with a task requiring continuous performance.
What does the task involve?
 Single digits appear in the centre of the screen, with 100 digits being shown per minute. A panel to the right of the central square displays the target sequences which participants must respond to. When the participant detects a sequence they must press a blue button at the bottom of the screen. There are 9 target sequences per minute.
Single digits appear in the centre of the screen, with 100 digits being shown per minute. A panel to the right of the central square displays the target sequences which participants must respond to. When the participant detects a sequence they must press a blue button at the bottom of the screen. There are 9 target sequences per minute.
Why this test
RVP tests sustained attention. This cognitive domain has been found to be impaired in depression.4
Cambridge Gambling Task
What does it test?
The Cambridge Gambling Task (CGT) was developed to assess decision making and risk taking behaviour outside a learning context.
What does the task involve?
 The task requires participants to decide whether a token will be hidden behind a red box or a blue box. Participants are then asked to bet a proportion of their points to support this decision. The odds of winning or losing are made explicit in the CGT by the ratio of red to blue boxes.
The task requires participants to decide whether a token will be hidden behind a red box or a blue box. Participants are then asked to bet a proportion of their points to support this decision. The odds of winning or losing are made explicit in the CGT by the ratio of red to blue boxes.
Why this test
As information from one trial does not inform the next in the CGT, limited demands are placed on learning and working memory processes, offering a clean measure of decision-making under risk. This presents CGT as a good option for investigating the impairments in decision-making under risk typically seen in depression14.
What research has been done and the need to improve:
Psychotherapy, notably cognitive behavioural therapy (CBT), has a strong evidence base in the treatment of depressive disorders8. In addition to face-to-face CBT, there is growing evidence to support remote therapist-led CBT, and guided self-help CBT8. Other types of therapy, including mindfulness based interventions are currently being tested for their effectiveness. A number of different pharmacological treatments, typically targeted to the serotonergic or noradrenergic system, have also been approved and widely adopted.
Despite these various treatment options, there is no universally successful intervention and patients experience both high rates of relapse and frequent persistence of cognitive symptoms after mood improves. Current research is focusing on treatments that can ameliorate cognitive impairment in mood disorders, in order to maximise long-term outcomes and quality of life, as well as, looking for objective markers capable of identifying, for a given individual the treatment options that are most likely to be effective and well-tolerated.
So why CANTAB?
Cognitive deficits are common in people with mood disorders, reflecting underlying dysfunction of monoamine neurochemical systems9, and of emotional processing circuitry10. Cognitive deficits represent core targets for existing and novel treatments11, 12. This battery of tests incorporates core domains often impaired in mood disorders, as well as those likely to be affected by interventions: sustained attention, delayed matching to sample (associative learning), spatial working memory, executive function, planning, emotional recognition and decision-making under risk.
CANTAB tests discriminate the neuropsychological profile of bipolar disorder from unipolar depression13, as well as effects of different medications in patients14. The battery avoids floor and ceiling effects that are common with other testing batteries in the field, by using carefully chosen ranged task-difficulties. Cognitive performance correlates with quality of life, even early in the course of bipolar disorder, making the battery not only biologically but also clinically relevant for mood disorders15.
References
1. Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry. 2004 Feb;49(2):124-38. Review.
2. Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014 Apr;43(2):476-93.
3. Murray CJL, Lopez AD, editors. The global burden of disease. Geneva: World Health Organization;1996
4. Rock, P. L. et al. ‘Cognitive Impairment In Depression: A Systematic Review And Meta-Analysis’. Psychological Medicine 44.10 (2013): 2029-2040. Web. 13 Oct. 2015.
5. Kellough JL, Beevers CG, Ellis AJ, Wells T. Time course of selective attention in clinically depressed young adults: An eye tracking study. Behavior Research and Therapy. 2008;46:1238–1243. doi: 10.1016/j.brat.2008.07.004.
6. Linde K, Rücker G, Sigterman K, Jamil S, Meissner K, Schneider A, Kriston L. Comparative effectiveness of psychological treatments for depressive disorders in primary care: network meta-analysis. BMC Fam Pract. 2015 Aug 19;16:103. doi: 10.1186/s12875-015-0314-x.
7. Grady MM, Stahl SM. Novel agents in development for the treatment of depression. CNS Spectr. 2013 Dec;18 Suppl 1:37-40; quiz 41.
8. Ressler KJ, Mayberg HS. Targeting abnormal neural circuits in mood and anxiety disorders: from the laboratory to the clinic. Nat Neurosci. 2007 Sep;10(9):1116-24.
9. Pringle A, Browning M, Cowen PJ, Harmer CJ. A cognitive neuropsychological model of antidepressant drug action. Prog Neuropsychopharmacol Biol Psychiatry. 2011 Aug 15;35(7):1586-92.
10. Clark L, Chamberlain SR, Sahakian BJ. Neurocognitive mechanisms in depression: implications for treatment. Annu Rev Neurosci. 2009;32:57-74.
11. Maalouf FT, Klein C, Clark L, Sahakian BJ, Labarbara EJ, Versace A, Hassel S, Almeida JR, Phillips ML. Impaired sustained attention and executive dysfunction: bipolar disorder versus depression-specific markers of affective disorders. Neuropsychologia. 2010 May;48(6):1862-8. doi: 10.1016/j.neuropsychologia.2010.02.015. Epub 2010 Feb 20.
12. Muralidharan K, Kozicky JM, Bücker J, Silveira LE, Torres IJ, Yatham LN. Are cognitive deficits similar in remitted early bipolar I disorder patients treated with lithium or valproate? Data from the STOP-EM study. Eur Neuropsychopharmacol. 2015 Feb;25(2):223-30.
13. Mackala SA, Torres IJ, Kozicky J, Michalak EE, Yatham LN. Cognitive performance and quality of life early in the course of bipolar disorder. J Affect Disord. 2014 Oct;168:119-24.
14. Clark L, Dombrovski AY, Siegle GJ, et al. Impairment in risk-sensitive decision-making in older suicide attempters with depression. Psychol Aging. 2011;26(2):321-330

